Glucose monitoring measurements in children with diabetes
Glucose monitoring measurements are important for tamariki and rangatahi with diabetes to:
- allow insulin adjustment
- detect high or low glucose levels so that treatment can be given if needed
- monitor and treat diabetes during exercise and illness
What you need to know about continuous glucose monitoring
Continuous glucose monitoring (CGM)
CGM are devices that monitor glucose levels in people with diabetes. They can also help you to see trends in your child's glucose levels. Most devices allow remote monitoring.
How the devices work
CGMs are inserted into the fatty layer under the skin. In CGM, a transmitter sends data constantly to a receiver, a compatible insulin pump or a smart device (such as a phone or tablet).
Sensor glucose readings are taken from interstitial fluid, not from blood. Interstitial fluid is the fluid that surrounds the cells of your tissue below your skin. Glucose moves from blood vessels and capillaries first and then into interstitial fluid. When rising or falling quickly (for example, after a meal or insulin), sensor glucose will be a bit behind the changes in glucose monitoring. So, it will almost always be a little different. It's important to check glucose levels by finger-prick if symptoms don't match sensor glucose, or you have concerns.
One of the real benefits of using continuous glucose monitoring with sensors is that it lets you see patterns and trends. Also, CGM allows families to set alarms for high and low glucose levels, which can be especially comforting overnight.
See side by side comparisons of glucose monitoring systems available in Aotearoa New Zealand.
Limitations of these devices
There can be some variation between the readings from continuous monitoring and blood glucose from finger-pricks. This difference depends on the individual and the device. There will be times when you need to confirm the result with a finger prick blood glucose check.
Finger prick glucose monitoring
Your diabetes team will train you to do finger prick glucose checking. Tamariki and rangatahi with type 1 diabetes will often be able to do this themselves. Finger prick checking is important for when your sensor glucose values don't seem to line up with symptoms of very low or very high glucose levels. You may also need to finger prick to calibrate the glucose sensor. Finger prick glucose levels are especially important when managing low glucose levels, or rapidly changing glucose levels. This is because sometimes the sensor glucose 'lag' actual glucose levels and so affect management.
Keep a record of glucose levels
Your diabetes team can see CGM glucose values because these are kept on secure databases. The team can view the values remotely, and can adjust insulin if needed. If you are finger pricking, the glucose values can be downloaded from the meter, or you could keep them in a diary. The team will check your diary values against what is recorded in the meter to check that they match up.
Depending on the treatment required, tamariki and rangatahi with type 2 diabetes may be able to monitor glucose levels less often.
Diabetes diary
The Clinical Network for Children and Young People with Diabetes has developed a 'diabetes diary'. It's for you to record your glucose levels. You can fill in your personal details, and it has guidance about hypo-management and sick day management as well.
To make it into a book, print double-sided on 'small edge'. You can also ask your diabetes team for a copy.
Source: New Zealand Child and Youth Clinical Networks
Target ranges for blood glucose levels
These are generally:
- before meals, 4 to 8 mmol/L
- after meals, 4 to 10 mmol/L
Your diabetes team may give you individualised targets. These may differ slightly to those above.
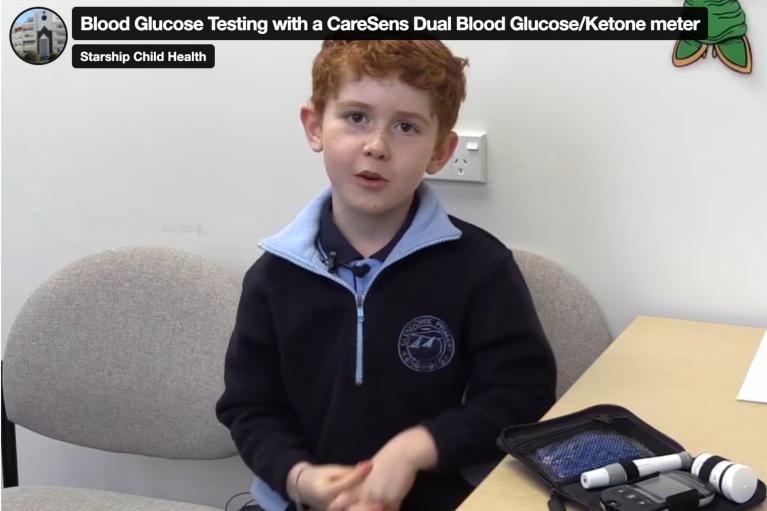
Check out a video about how to do a blood glucose finger prick test at the Starship website. There is more information and videos about glucose monitoring.
Acknowledgements
The content on this page has been approved by the Clinical Network for Children and Young People with Diabetes, Paediatric Society of New Zealand.
