Key points about tube feeding
- tube feeding helps tamariki who are not able to eat or drink enough by mouth
- tube feeding helps these tamariki meet their nutritional needs
- tamariki who can't safely swallow liquids, foods, or medicines may need tube feeding
- it is possible for you and your whānau (family) to learn how to use the feeding tube safely at home
- it can be difficult to know how long tamariki will need a feeding tube for
- most tamariki can stop tube feeding when it is no longer medically required
- prolonged tube feeding refers to tube feeding for longer than 3 months
- tube feeding will not limit your child from being able to do most of their usual activities
- your child may see a range of health professionals while they are having tube feeding
If you are new to tube feeding at home, start with the tube feeding checklist, and keep it somewhere visible.
Tube Feeding - Checklist For Tube Feeding At Home
What is tube feeding?
Tube feeding involves delivering liquid feed through a tube. This can be through the nose (nasal tube) or stomach (gastrostomy tube).
Feed types include expressed breast milk, formula or a specialised liquid feed.
Nasal tubes for tube feeding
An illustration showing a child with a feeding tube.
Source: KidsHealth
There are 2 types of nasal tubes:
- nasogastric (NG) tubes
- nasojejunal (NJ) tubes
Nasogastric or NG tubes
A nasogastric or NG tube is a soft polyurethane tube. A doctor or nurse will put the tube in. It goes through the nose, down the food pipe (oesophagus) and into the stomach.
Nasojejunal or NJ tubes
A nasojejunal or NJ tube goes into the nose, down through the stomach and ends in the jejunum. The jejunum is part of the small intestine. Tamariki may need an NJ tube if they cannot tolerate feeding to the stomach.
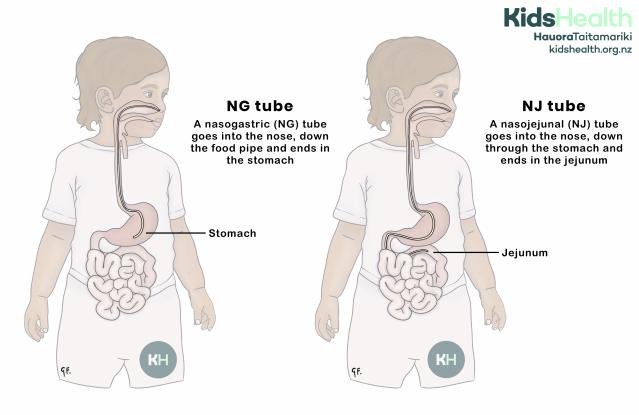
An illustration showing an NG tube ending in the stomach and an NJ tube passing through the stomach and ending in the jejunum.
Source: KidsHealth
transcribeTranscript
This illustration compares two types of nasal feeding tubes.
- On the left, an NG tube (nasogastric tube) goes into the nose, down the food pipe, and ends in the stomach.
- On the right, an NJ tube (nasojejunal tube) goes into the nose, passes through the stomach, and ends in the jejunum, which is part of the small intestine.
At the top of the illustration is the KidsHealth logo with the website: kidshealth.org.nz.
Will my child need an operation to have a nasal tube put in?
Your child will not need an operation. Nasal tubes are usually put in by a nurse. Nasal tube feeding is a temporary way of feeding.
Things to know about nasal tubes
- you will need to tape the nasal tube to your child's cheek - this may irritate them
- your child may pull the tube out, but you can learn how to replace the tube at home
- you will need to change your child's tube regularly
- your child may have more reflux or gagging, and they may refuse to eat by mouth
- for longer term tube feeding the doctor may replace the nasal tube with a gastrostomy tube
- your health professional will provide further information to help deal with any issues
Gastrostomy tubes for tube feeding
A gastrostomy tube goes directly into your child's stomach from the skin of your child's tummy.
The doctor may put the tube in during an operation, or by a procedure called endoscopy. Endoscopy is a way of looking inside the digestive tract. It uses a flexible tube, an endoscope, with a small camera on the end of it. The endoscope goes into your child's mouth, down the food pipe (oesophagus), and into the stomach. Your child will need to recover in hospital for a few days after the gastrostomy tube goes in.
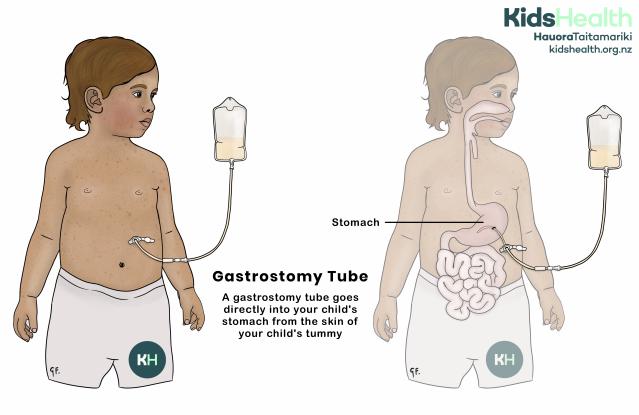
An illustration showing a child with a gastrostomy tube going directly into the stomach through the tummy, with a feeding bag attached.
Source: KidsHealth
transcribeTranscript
This illustration shows a child with a gastrostomy tube.
- The tube goes directly into the child’s stomach through an opening in the skin of the tummy.
- A feeding bag is attached to the tube outside the body to give milk or liquid food.
At the top of the illustration is the KidsHealth logo with the website: kidshealth.org.nz.
Types of gastrostomy tubes
Your child's health professional will discuss the best type of tube with you.
Types of gastrostomy tubes include:
- retention disk PEG
- PEG-J
- balloon gastrostomy
- MicKey button
Things to know about gastrostomy tubes
Gastrostomy tubes are a safer and more comfortable long-term option.
Replacing gastrostomy tubes
You may be able to replace some tubes at home with training from your health professional.
Tubes generally need to be replaced:
- every 6 months for balloon inflated gastrostomy and MicKey tubes
- between 2-5 years for retention disk PEG and PEG-J tubes
If there is any deterioration of the tube or it is not working properly, it may need replacing sooner.
Healing after insertion
During the healing process you may notice skin changes. Red, bubbly tissue (granulation tissue) may form around the skin where the tube goes in. This is not dangerous and your health professional can treat this with ointment.
Blocked gastrostomy tube
Gastrostomy tubes may become blocked by food or some medications. Ask your health professional before putting unprescribed foods or medications down the tube.
If your child's gastrostomy tube becomes blocked, contact your health professional. They may get you to try to unblock it with extra water flushes.
Tube feeding plans
Your child's dietitian or paediatrician (child health specialist) will give you a feeding plan for your child. This will include timings and types of feed. The type of feeding plan will depend on your child's medical condition and how much feed they can handle. Specialised liquid feeds are only available on prescription from a dietitian or doctor.
There are 2 ways you can feed your child:
- bolus feeds - larger amounts of liquid feed given at set times over the day so that it's like meal times
- small amounts given continuously by a feeding pump
Health professionals involved with tube feeding
There will be a range of professionals supporting you and your child with tube feeding. These professionals may also help your child begin to change to oral feeding. Tube feeding involves a range of professionals, called a multidisciplinary team. This is because there are many different factors that contribute to feeding.
Your child's multidisciplinary team may include:
- family doctors (GPs)
- paediatricians
- children's community nurses
- dietitians
- speech language therapists
- psychologists
- occupational therapists
The impact of tube feeding on children and their family
Tube feeding takes some adjustment. But, many whānau report relief after their child starts tube feeding. They see their child getting the nutrition, liquid (hydration) or medication they need.
With the help of your health professionals, you will be able to learn to use the feeding tube safely at home. If safe, your child will still be able to eat by mouth (orally) while they have a feeding tube.
Your child will still be able to take part in most activities such as:
- tummy time
- play
- swimming
- daycare or school
People who care for your child can also learn to use the feeding tube. Ask your child’s healthcare team about travel, swimming, and training other carers.
It is a good idea to have some prepared responses to questions people and other tamariki may ask about the tube. This could be questions such as:
- What is it for?
- Why is it there?
You may find it emotionally overwhelming during some periods of your tube feeding journey. Especially in the first weeks at home, or when your child transitions to long-term tube feeding. It is helpful to get support from your feeding team, other professionals, or parents. You can ask your health professionals if there are support groups in your area.
How long is tube feeding needed
Your child will need to tube feed until they can eat or drink enough by mouth to meet their nutritional needs. Some tamariki with certain medical conditions may always need some tube feeding.
To be ready for feeding by mouth (oral feeding), your child will need to:
- show that they can swallow safely
- be otherwise medically stable
If your child doesn’t have other medical conditions and is safe to eat, talk to your health professional. Ask about early support and a plan to work up to oral feeding.
Helping children go from tube feeding to feeding by mouth
Planning
It is helpful to plan for feeding by mouth with your health professionals as early as possible. You may start to include 'mealtime' experiences into your child's tube feeding routine. There are several different ways to try this.
Give tube feeds in a food context
For a younger child, this could be while cuddled up with you. For older tamariki, it could be at a small table with finger food or in a highchair with the whānau at dinner time.
Encourage tube feeding by other people and at other places
This could be by grandparents in their kitchen. Or at a close friend or family member's house. Think of the ways that tamariki eat with different people and in different places.
Involve your child in mealtime preparation and other food experiences
Involve your child in birthday parties, visits to cafes and restaurants.
Encourage your child to explore food
Encourage your child to explore food through their senses. Let them touch, smell and look at their food.
Consider changing from a nasal tube to a gastrostomy tube
Changing early can minimise the discomfort to the mouth, face and swallowing caused by nasal tubes. You may also have more time to help your child build skills for oral eating.
General Mealtime Strategies To Support Your Child Going From Tube Feeding To Oral Feeding
Approaches for tube weaning and changing to feeding by mouth
Seek guidance regularly from your health professionals. They will guide you on when your child may be ready to change from tube feeding to feeding by mouth (oral feeding).
Moving From Tube Feeding To Oral Feeding
More information and support

A New Zealand Facebook group for families that have a tube-fed child (or have had a tube-fed child at some stage). Please remember that this Facebook group is not moderated by health professionals. The advice is often from parents or members of the public. Before making changes to your child's feeding regime, talk with your child's healthcare team.
Acknowledgements
The content on this page has been developed and approved by the Clinical Network for Paediatric Tube Feeding, Paediatric Society of New Zealand | Te Kāhui Mātai Arotamariki o Aotearoa.
